Antimony Trioxide
Antimony Trioxide Profile

INDUSTRIAL CHEMICALS – POSSIBLE CARCINOGEN (IARC 2B)
Contents
Antimony Trioxide Profile
General Information
Antimony trioxide (Sb2O3) is a slightly soluble, white crystalline powder.[1] It is produced by smelting antimony-containing ores[1] or reacting antimony trichloride with water.[2] Antimony is not abundant in the earth’s crust.[3] Antimony trioxide may also be referred to as diantimony trioxide (DAT), antimony oxide, or in manufacturing as antimony white.[4] There are numerous other synonyms and product names; see the Hazardous Substances Data Bank (HSDB) for more information.[4]
Antimony trioxide was last classified by the International Agency for Research on Cancer (IARC) in 1989 as Group 2B, possibly carcinogenic to humans, based on inadequate evidence in humans and sufficient evidence in animals.[1] Antimony trioxide is a respiratory carcinogen in female rats.[1]
The epidemiological literature on exposure to antimony trioxide is not extensive and is limited by difficulty in controlling for confounding variables. Recent reviews of studies report excesses of lung cancer in antimony exposed smelter workers, but factors such as smoking, exposures to PAHs and other metals (e.g. arsenic), were not appropriately controlled.[2,5]
Antimony trioxide has also been linked to pneumoconiosis, bronchitis, and airway inflammation.[3] Digestive and neurologic symptoms have been reported from high levels of exposure, but causal relationships have not been established.[3] An early study reported that exposure is associated with an increase in spontaneous abortions, premature birth, and slow growth rates in offspring.[6] The study’s control of confounding variables and exposure assessment techniques, however, were unclear.[7]
Regulations and Guidelines
Occupational exposure limits (OEL)[8,9,10,11,12,13,14,15,16,17,18,19,20,21,22]
| Canadian Jurisdictions | Substance | OEL (mg/m3) |
|---|---|---|
| Canada Labour Code | Sb2O3, production Sb & its compounds | ALARA 0.5 |
| AB | Sb2O3, production Sb & its compounds | – 0.5 |
| BC, MB, ON, NB, NL, PEI, NS | Sb2O3, production Sb & its compounds | ALARA 0.5 |
| SK, NT, NU | Sb2O3 Sb & its compounds | – 0.5; 1.5 [stel] |
| QC | Sb2O3 Sb & its compounds Sb2O3 production (as SB) | 0.5 0.5 ALARA |
| YT | Sb2O3 production (as SB) | 0.5 0.5; 0.75 [stel] |
| Other Jurisdictions | Substance | OEL (mg/m3) |
| ACGIH 2020 TLV | Sb2O3, production Sb & its compounds | ALARA 0.5 |
mg/m3 = milligrams per cubic meter
ALARA = as low as reasonably achievable
stel = short term exposure limit (15 min. maximum)
ACGIH = American Conference of Governmental Industrial Hygienists
TLV = threshold limit value
Canadian environmental guidelines and standards*
| Jurisdiction | Limit | Year |
|---|---|---|
| Canadian and Ontario Drinking Water Guidelines (Antimony) | 0.006 mg/L | 2017[23] 2016[24] |
| BC’s Contaminated Sites Regulation, BC Reg 375/96 | Sets soil standards for the protection of human health for antimony: Agricultural and low density residential sites: 250 μg/g Urban park and high density residential sites: 500 μg/g Commercial sites: 1,500 μg/g Industrial sites: 40,000 μg/g
Drinking water: 6 μg/L | 2017[25] |
| Ontario Ambient Air Quality Criteria | Annual: 0.12 µg/m3 24-hour: 0.6 µg/m3 | 2016[26] |
| Ontario’s Air Pollution – Local Air Quality Regulation Standards | 24-hour standard: 25 µg/m3; Prohibited discharge into the air if the concentration of antimony trioxide exceeds the standard | 2020[27] |
| Quebec’s Clean Air Regulation | 1 year limit: 0.17 µg/m3 (antimony, metal and compounds); Prohibited discharge into the air if the concentration of antimony trioxide exceeds the standard | 2011[28] |
*Standards are legislated and legally enforceable, while guidelines (including Ontario ambient air quality criteria) describe concentrations of contaminants in the environment (e.g. air, water) that are protective against adverse health, environmental, or aesthetic (e.g. odour) effects
Canadian agencies/organizations
| Agency | Designation/Position | Year |
|---|---|---|
| Health Canada | DSL – high priority substance (greatest potential for exposure) | 2006[29] |
| Challenge to Industry | Batch 9 | 2010[30] |
| National Classification System for Contaminated Sites | Rank = “High hazard”, potential human carcinogen (antimony) | 2008[31] |
| Cosmetic Ingredient Hotlist | Not permitted | 2004[32] |
| PMRA List of formulants | List 4B: List 4B contains formulants, some of which may be toxic, for which there are sufficient data to reasonably conclude that the specific use pattern of the pest control product will not adversely affect public health and the environment | 2018[33] |
| Environment Canada’s National Pollutant Release Inventory | NPRI Part (Threshold Category): 1A, Reportable to NPRI if manufactured, processed, or otherwise used at quantities greater than: 10 tonnes (for antimony and its compounds) | 2016[34] |
DSL = domestic substance list
Antimony trioxide was not included in other Canadian government guidelines, standards, or chemical listings reviewed.
Main Uses
Antimony trioxide is mainly used as a chemical synergist in chlorinated and brominated flame-retardants, increasing the retardants’ effectiveness.[35] Flame retardants containing antimony trioxide are used widely in producing textiles, plastics, rubber, and paints.[1]
Antimony trioxide is the main catalyst used to produce polyethylene terephthalate (PET) and polyester fibers. PET is commonly used in plastic packaging for water and soft drinks.[35] It is also used as a pigment and/or clarifying agent in certain glasses and ceramics.[36] As of 1995, antimony trioxide gained popularity as an additive in optical glass, replacing arsenious oxide.[37]
Antimony metal increases hardness and strength in lead alloys and is used in lead storage batteries, solder, sheet and pipe metal, bearings, castings, and pewter.[3] Antimony trioxide is produced when elemental antimony is heated and/or oxidized.[3]
Canadian Production and Trade
Antimony trioxide is primarily used to create household flame retardants and plastic (polyethylene terephthalate).[38]
Antimony is naturally occurring in the Cordilleran (west coast) and Appalachian (east coast) regions of Canada.[39] Approximately 401 tonnes of antimony is mined in Canada annually, and it is considered a “critical mineral for the economic success of Canada”.[39,40] China, Belgium and France are the highest exporters globally, each exporting over 10,000 tonnes annually.[41]
At full capacity, Beaver Brook Antimony Mine Inc. in Newfoundland will mine approximately 160,000 tones of antimony per year.[42,43] Operations were temporarily suspended in November 2020 due to the COVID-19 pandemic however mining resumed at the end of September 2021.[42]
Production and trade
| Activity | Quantity | Year |
|---|---|---|
| Canadian Production | 76 t | 2013[44] |
| Export: | 109 t (of ‘antimony oxides’) | 2021[45] |
| Import: | 2,395 t (of ‘antimony oxides’) | 2021[45] |
t = tonne
Environmental Exposures Overview
The main source of exposure to antimony trioxide for the general population is through dermal contact with household items that contain flame retardants, such as paint, mattress covers and furniture upholstery.[46] However, Environment Canada reports that exposures from this pathway are low.[46]
Other sources of environmental exposure include food, drinking water, and air.[3,46] Overall, levels of antimony trioxide in water are low due to its poor solubility in water.[46] Higher levels of exposure may occur around smelters, incinerators, and near combustion of petroleum and coal products.[3] Higher levels of exposure to antimony trioxide have also been associated with smokers and those exposed to secondhand smoke.[47]
Searches of Environment Canada’s National Pollutant Release Inventory (NPRI) and the US Consumer Product Information Database yielded the following results on current potential for exposure to antimony trioxide in Canada:
NPRI and US Consumer Product Information Database
| NPRI 2015[48] | ||
|---|---|---|
| Substance name: ‘Antimony and its compounds’ | ||
| Category | Quantity | Industry |
| Released into Environment | 2.9 t | Non-ferrous metal (except aluminum) production and smelting, petroleum and coal product manufacturing, Metal ore mining, Other electrical equipment manufacturing, oil and gas extraction (46 facilities) |
| Disposed of | 508 t | |
| Sent to off-site recycling | 184 t | |
t = tonne
| US Consumer Products 2016[49] | ||
|---|---|---|
| Search Term | # Products | Product Type |
| ‘Antimony oxide’ | 26 | Insulation (solid or fibre form) |
Occupational Exposures Overview
Inhalation is the most important route of occupational exposure, however oral and dermal contact are also a concern.[3]
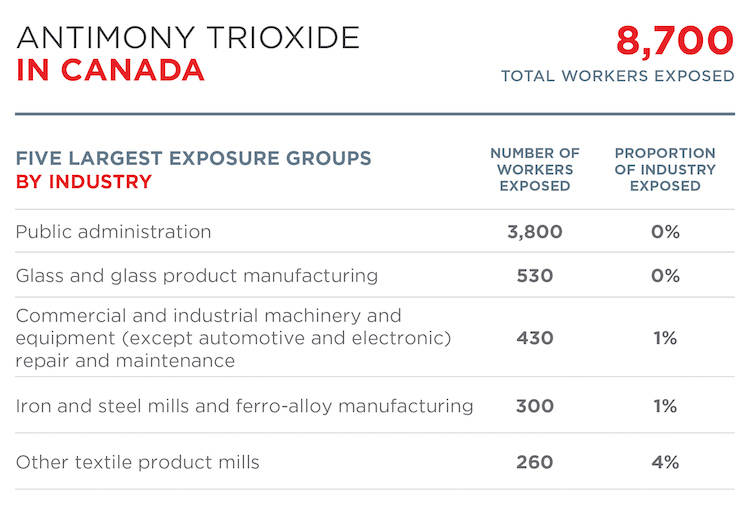
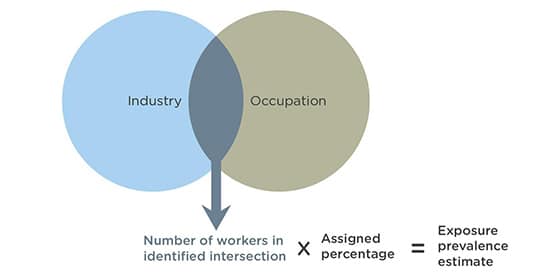
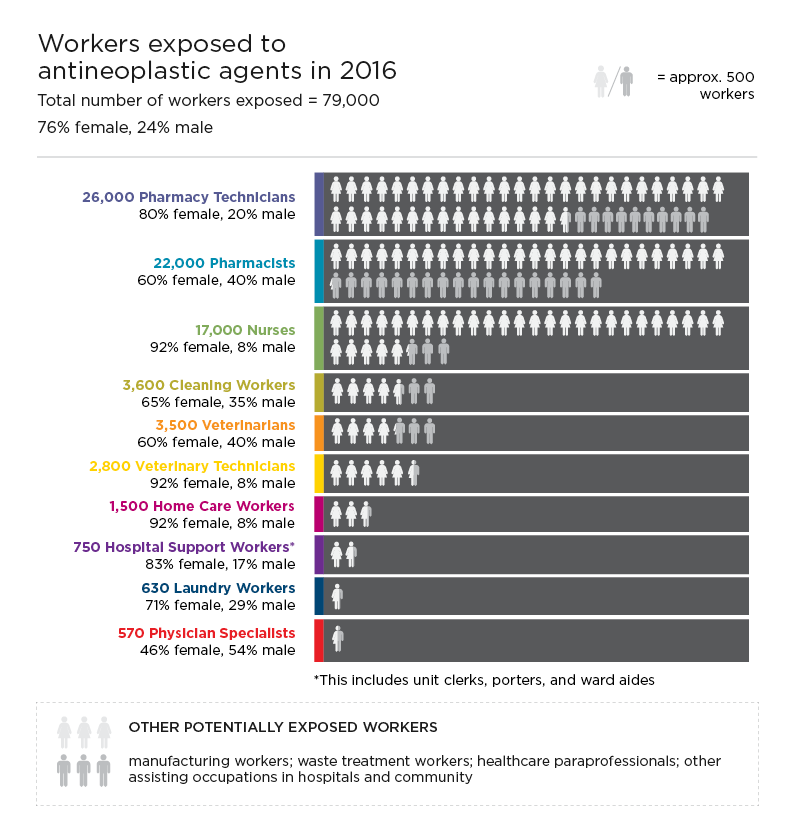
CAREX Canada estimates that approximately 8,700 Canadians are exposed to antimony trioxide in the workplace. The primary industrial groups exposed are public administration, followed by glass and glass product manufacturing. In terms of occupations, the largest exposed groups are police officers (exposed in firing ranges), welders and related machine operators, artisans and craftspersons, and glass forming and finishing machine operators and glass cutters.
Other workers likely to be exposed include those involved in: antimony trioxide production; antimony processing, smelting, and packaging of antimony compounds; production of ceramics and alloys that contain Sb2O3; and manufacture and application of flame retardants.[36]
Workers in facilities that recycle lead-acid batteries may also be exposed to antimony.[50] Firefighters and other emergency workers may be exposed when materials containing antimony trioxide as a fire retardant combust.[36] Exposures may also occur for workers involved producing PET bottles, where antimony trioxide is used as the main catalyst.
For more information, see the occupational exposure estimate for antimony trioxide.
Sources
Photo: Wikimedia Commons, Rob Lavinsky
Other Resources
- Agency for Toxic Substances and Disease Registry (ATSDR). ToxFAQs Sheet: Antimony (1995)
- Shotyk W, Krachler M, Chen B. “Contamination of Canadian and European bottled waters with antimony from PET containers.” J Environ Monit 2006;8:288-292.
- Krachler M, Zheng J, Koerner R, Zdanowicz C, Fisher D, Shotyk W. “Increasing atmospheric antimony contamination in the northern hemisphere: snow and ice evidence from Devon Island, Arctic Canada.” J Environ Monit 2005;7:1169 – 1176.
Subscribe to our newsletters
The CAREX Canada team offers two regular newsletters: the biannual e-Bulletin summarizing information on upcoming webinars, new publications, and updates to estimates and tools; and the monthly Carcinogens in the News, a digest of media articles, government reports, and academic literature related to the carcinogens we’ve classified as important for surveillance in Canada. Sign up for one or both of these newsletters below.
CAREX Canada
School of Population and Public Health
University of British Columbia
Vancouver Campus
370A - 2206 East Mall
Vancouver, BC V6T 1Z3
CANADA
As a national organization, our work extends across borders into many Indigenous lands throughout Canada. We gratefully acknowledge that our host institution, the University of British Columbia Point Grey campus, is located on the traditional, ancestral, and unceded territories of the xʷməθkʷəy̓əm (Musqueam) people.